
Blue cross blue shield copay medical code 99211 software#
*Policy sources include, but are not limited to, AMA and CMS policy regarding reimbursement of E/M services submitted with Modifier 25, as well as EmblemHealth’s plan-specific requirements (refer to the Claims Review Software section of the Claims chapter of the EmblemHealth Provider Manual for additional information about claims review software used by EmblemHealth).
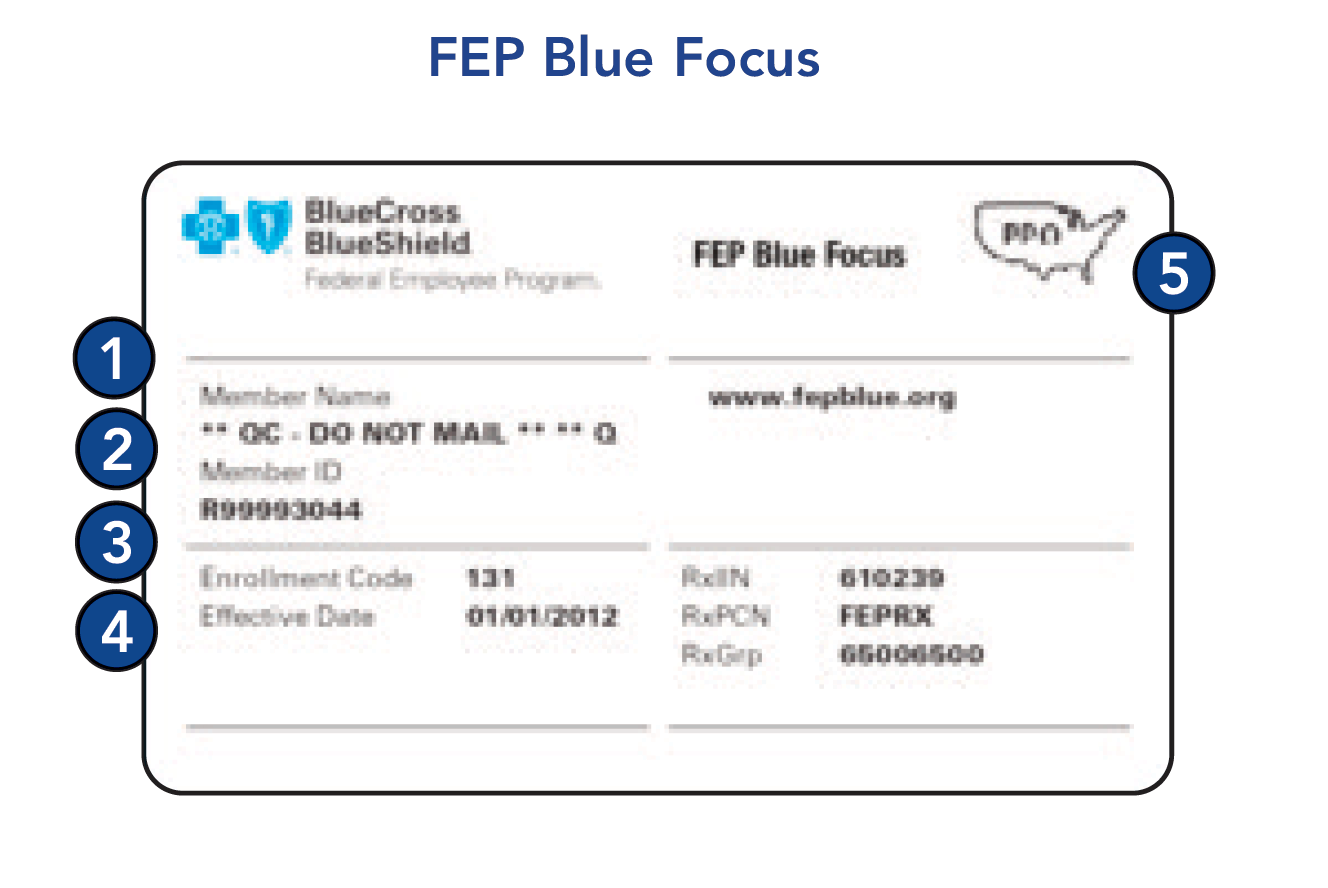
CPT codes 8103 will not be separately reimbursed unless Modifier 25 is appended to the E/M service indicating that a diagnostic, non-screening, urinalysis was performed. And it is my job to make sure that I get my providers the highest reimbursement possible.As noted in the Provider Manual, EmblemHealth uses multiple types of commercially available claims review software to support the correct coding of claims that result in fair, widely recognized and transparent payment policies.* One of these policies bundles CPT code 81002 and CPT code 81003 (Urinalysis, by dip stick or tablet reagent) when reported with an Evaluation and Management service (e.g., CPT codes 99201-99205, 99211-9921-99397). This policy addresses Blue Cross and Blue Shield of Minnesota’s (Blue Cross) coverage and. Typically, five minutes are spent performing or supervising these services. Office visit, established patient, low to moderate severity. He has a 25 copay for office visits, so that is what he’ll pay for this visit. Usually the presenting problem is minimal. Mike has met his deductible, and he doesn’t have coinsurance. Getting your provider paid for at least the 90460 and one 90461 will be a higher reimbursement than billing with an incorrect code. CPT 99211 is an office or other outpatient visit for the Evaluation and Management (E&M) of an established patient that may not require the presence of a physician. AND a copay gets applied that you’ll most likely end up waiving anyway. If the vaccine is administered with no counseling, you would use the regular 9042 codes for your intramuscular administrations.Īs an additional consideration, the 99212 gets paid a very small amount anyway. An acute, uncomplicated illness at time of visit. You can use 9041 for vaccines administered intramuscularly, nasally, or orally. Bill 99213 (or 99203 for new patients) with preventive or wellness code. MHK Reminder Medical Records Cover Sheet Reminder COVID Vaccine Policies Cost Share Waiver for Treatment of Confirmed Cases of COVID-19 Pulse Oximeters OTC Medicare Benefit. These codes are also nice because they do not specify the method of administration. Blue Cross & Blue Shield of Rhode Island 2021 Updates MaPresented by: Stef Vito. You would use code 90460 for the first vaccine and 90461 for any subsequent vaccines. For pediatricians, there is a code that includes the administration of vaccines and the time spent counseling the patient/guardian. However, the office does deserve to be reimbursed for any time spent counseling. Blood pressure checks, ear lavages, EKGs, vaccinations, that sort of thing. Anything the patient comes in for that does not require the presence of the physician can be a 99211.

In fact, there are no specific requirements. The requirements for a 99211 are incredibly broad. And counseling only does not include an exam or any decision making. While the MA’s can take the history, the only person medically qualified to do an exam or any medical decision making is a provider. billed with Evaluation & Management (E&M) CPT codes (99201-99205 99211-99215) applicable to the. The requirements for a 99212 include a problem focused history, a problem focused exam, and straightforward medical decision making. E&M University has an excellent breakdown of the requirements for each of the codes.

Well, short story shorter, the only office visit we can bill when the provider does not see the patient is a 99211. My colleague’s question was whether or not a 99212 would be acceptable to report to the insurance company in that manner. CPT codes 8103 will not be separately reimbursed unless Modifier 25 is appended to the E/M service indicating. HealthPlan has contracted with Amerigroup Partnership. One of these policies bundles CPT code 81002 and CPT code 81003 (Urinalysis, by dip stick or tablet reagent) when reported with an Evaluation and Management service (e.g., CPT codes 99201-99205, 99211-9921-99397). Since the medical assistants spent some time counseling the patient, the doctor wanted to make sure the practice was paid for that time. BlueChoice HealthPlan is an independent licensee of the Blue Cross Blue Shield Association. One of her providers, a pediatrician, wanted to bill a 99212 with vaccines even when the patient did not see the doctor. The Evaluation and Management (E/M) CPT code 99211 is probably the most overused and abused service billed to Medicare. A few weeks ago, a colleague gave me an interesting dilemma.


 0 kommentar(er)
0 kommentar(er)
